Before and after photos on complications and problems in periodontics performed in our Gum Disease Treatment office.

This photo documents periodontal complications from using Calcium Channel blockers without dental clearance. Calcium Channel blockers are commonly used to treat high blood pressure, angina pectoris and coronary artery disease. These medications should NOT be prescribed by physicians until periodontal health has been achieved and confirmed by a dentist. Physicians should obtain periodontal clearance before prescribing such medication.
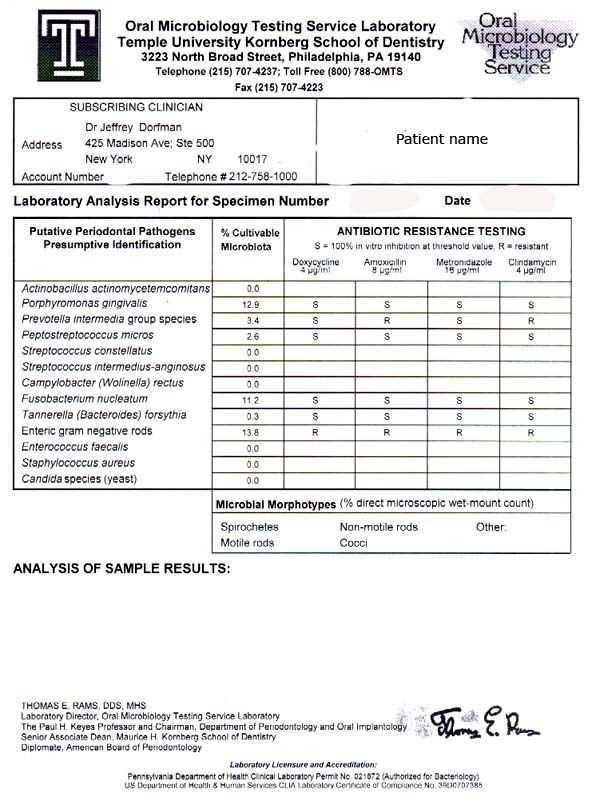
Oral Microbiology test results for a 41 year old female with severe periodontal disease who did not favorably respond to three years of Periostat Doxycycline antibiotics treatment at another dental office. Enteric gram negative rods, which populated 13.8% of the culture, are shown to be resistant to Doxycycline. This patient was successfully treated with Amoxycillin & Metronidazole antibiotics. She was also referred to a nutritionally oriented physician, Keith Berkowitz, MD (NYC), where a fasting glucose tolerance test showed her to be diabetic.

A complicated periodontal differential diagnosis. A 50 year-old female presented with itching of buccal gingiva gums on the upper left and right jaws. The red lesions and the itching have been present for months. No bone loss, no skin conditions, no ocular conditions. Periodontal Differential Diagnosis: 1. Non-specific dermatitis – patients mother had a dermatologic condition, or 2. Viral – patient has recurrent herpes. Treatment: We prescribed Kenalog. If her condition improved, it confirmed the first diagnosis. If it gets worse, consider Diagnosis #2. If no change, then change topical steroid. The patient’s symptoms improved with Kenalog.
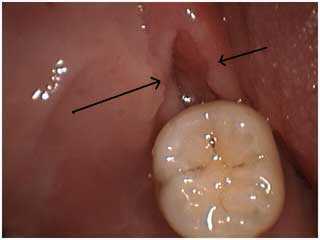
Periodontal problems: dealing with a recurring pericoronitis. The Periodontist performed a distal wedge procedure – one week post op. This periodontal surgery is performed to remove gum tissue – the pericorium – that may grow over the biting surface of the lower back molar teeth. The pericorium in this patient had occasionally become infected and the swollen gum pain required antibiotics.
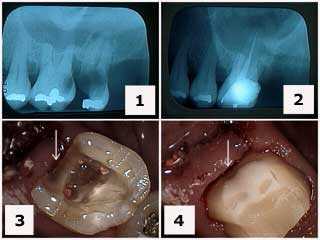
Periodontal surgery is sometimes needed on healthy gums, unhealthy teeth. A molar with severe dental caries, tooth decay. 1) Initial x-ray. 2) X-ray following tooth extraction of #15 and root canal therapy on tooth #14. Note the gingival extent of the tooth decay – below the gum line. 3) Tooth preparation following root canal therapy and the removal of the distal tooth cavity. 4) Final tooth preparation of the composite crown build-up. Note how the distal tooth preparation extends gingivally beyond the composite to tooth.
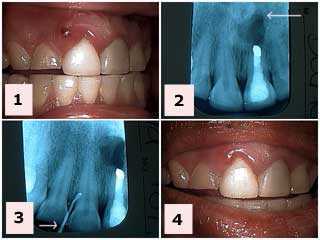
Acute periodontal abscess that caused swollen gum pain. 1) This patient presented with this gum fistula between tooth #’s 7 & 8. Tooth #’s 8 & 9 had acrylic laminate veneers placed about two years ago by her local dentist. Her general dentist had performed a gingivectomy – minor gum surgery – last year to attempt to treat the occasional swelling of the gums in this same area. 2) The x-ray of tooth #9 shows a healed apicoectomy from 12 years ago that is not related to the current problem. 3) A gutta percha point was placed in the fistula gum boil and radiographed to see where it went. It stayed at the coronal gingiva gum around the margin of the laminate veneer. The patient was put on tetracycline antibiotics for a week. [This is not a recommendation for everybody!] 4) Reevaluation two days later showed improvement in symptoms, gum pain relief and gingival inflammation. An evaluation by the Periodontist and recontouring of the laminate veneer margin will occur following resolution of the acute condition.

Acute periodontal abscess that caused swollen gum pain. This patient presented with this draining fistula between tooth #’s 7 & 8. Tooth #’s 8 & 9 had acrylic laminate veneers placed about two years ago by her local dentist. Her general dentist had performed a gingivectomy – minor gum surgery – last year to attempt to treat the occasional swelling of the gums in this same area. A gutta percha point was placed in the fistula gum boil and x-rayed to see where it went. It stayed at the coronal gingiva around the gum margin of the laminate veneer. The patient was put on tetracycline antibiotics for a week. [This is not a recommendation for everybody!]. Reevaluation two days later showed improvement in symptoms, gum pain relief and gingival inflammation. An evaluation by the Periodontist and recontouring of the laminate veneer margin will occur following resolution of the acute condition of the periodontia.

Acute periodontal abscess that did not cause gum pain. This patient had not been to the dentist for over two years. The xrays look normal. He received a dental prophylaxis teeth cleaning and was placed on a chlorhexidene mouthwash. He was rescheduled for scaling and root planing and then further reevaluation of the periodontium with the Periodontist.

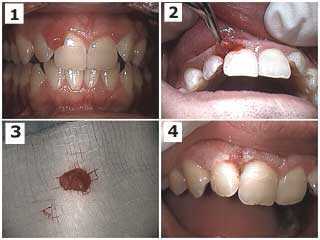
Treatment of a periodontal complication on an upper front tooth #9. 1) & 2) Pre-operative photograph and x-ray. Note the angular bony defect in the radiograph. The patient reported that the tooth was getting longer and that he never previously had the tooth gap space between his two front teeth. 3) Palatal photo of the teeth splint placed between teeth #’s 8 & 9. 4) Post-operative photo one hour later. Dental bonding placed between the teeth to close the teeth gap space also hides the palatal wire splint. The incisal edge of tooth #9 was shortened and the occlusion – teeth bite – was checked and adjusted for fremitus. Root planing was next performed and the patient placed on a three-month periodontal reevaluation.
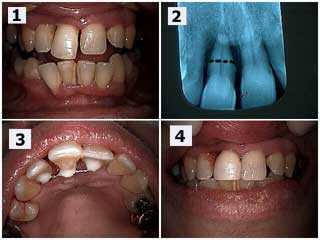
Periodontal complication for an upper right front tooth #8 that was very loose and the patient wanted to save it for as long as possible. 1) Upper right central incisor (#8) has extruded – grown down – and moved labially – toward the lip – and a diastema – tooth gap space – has resulted. 2) The x-ray shows severe bone loss. The black dotted line shows the location for a potential root resection – cutting the root off – if necessary. Root planing was performed after the teeth splint was placed and the patient will return in three months to reevaluate periodontal healing and the potential need for the root resection. 3) Palatal photo of the splint between teeth #’s 7 – 9. 4) Post-op view. Same day. Notice the diastema space was closed with bonding to hide the splint and the incisal edge of #8 was shortened.

Gingival gum recession around an old dental crown margin. This can make the tooth very sensitive to symptoms such as: touch, air and/or hot & cold liquids. Treatment depends upon the severity of the subjective symptoms and can range from: 1) do nothing and reevaluate, 2) using desensitizing agents, 3) periodontal gum surgery or 4) remaking the crown with or without root canal therapy. It is better to be conservative.
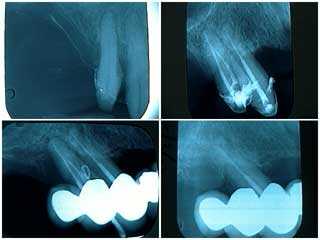
Periodontal complications. These radiographs x-rays show of a failing distal tooth abutment in a one year old ten teeth dental bridge. 1) Pre-operative xray. 2) Following root canal therapy, root planing and open flap periodontal debridement. 3) Gutta percha placed into a periodontal abscess one year later. 4) Following root planing, targeted antibiotics and tooth extraction. The roots of this extracted tooth were fused. This patient was scheduled for a three month recall; she did not return for eight months following her first three month recall visit. The periodontal abscess was readily apparent at this time. It is suggested that oral reconstruction patients are treated, not cured, and that they must be closely supervised. Patients need to be acutely aware of the need for frequent recall visits. It is possible that earlier diagnosis and intervention might have prevented the loss of this tooth. Follow up – this ten teeth dental bridge has been stable for nine years since this procedure.

How to remove a failing distal abutment tooth from under a large porcelain fused to metal dental bridge without removing or damaging the bridge. 1) Upper first premolar with probing to the tooth root apex. 2) Horizontal sectioning through the tooth to separate it from the dental bridge. You need to reduce enough of the remaining tooth root to elevate it while under the bridge. 3) Tooth socket after tooth removal. 4) Extracted tooth root. The gingival gum surface of the newly created pontic could be received dental bonding if necessary after primary healing has occurred. Creative periodontics.

Periodontal complication: combined occlusal – periodontal bite – gum problems. This patient’s front teeth are moving out and down and she now has a front teeth gap space. Fremitus – movement of tooth #8 upon biting her teeth together – was noted. Also notice her deep bite. Consider incisal adjustment of the lower front teeth. Next, periodontal root planing and scaling and then probably gum surgery in the upper anterior. Following gum healing consider dental bonding with a palatal splint after incisal reduction of tooth #8.

Pyogenic granuloma on the papilla between two teeth of a 40-year-old male. The radiographs reveal no pathology. The tissue was firm and did not respond to scaling and root planing. There was not tooth or gum pain and it did not bleed upon probing. Initial diagnosis: irritation fibroma. The tissue was sent for biopsy; the pathology report indicated it was a pyogenic granuloma. Photo 1 of 3.
Pyogenic granuloma on the papilla between two teeth of a 40-year-old male. The radiographs reveal no pathology. The tissue was firm and did not respond to scaling and root planing. There was not tooth or gum pain and it did not bleed upon probing. Treatment: surgical excision. The tissue was sent for biopsy; the pathology report indicated it was a pyogenic granuloma. Photo 2 of 3.

Pyogenic granuloma on the papilla between two teeth of a 40-year-old male. The radiographs reveal no pathology. The tissue was firm and did not respond to scaling and root planing. There was not tooth or gum pain and it did not bleed upon probing. Treatment: surgical site after excision and placement of Coe-pak periodontal wound dressing. The tissue was sent for biopsy; the pathology report indicated it was a pyogenic granuloma. Photo 3 of 3.

Periodontal complications in a full mouth oral reconstruction dental fear phobia patient. How to treat the periodontal disease? Creative periodontics. First treat the fear.
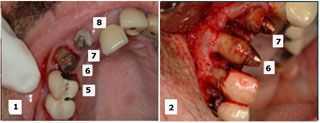
Periodontal complications. Selective teeth extractions during an upper oral reconstruction. The initial treatment plan considered saving teeth #’s 6, 7 and 9 while extracting teeth #’s 5 and 8. During the periodontal surgery, tooth #5 was considered more stable than #6 so #5 was retained and #6 was extracted. The retained teeth will be used to support a fixed temporary dental bridge until subsequent implant dentistry is completed.