Before and after photos on X-rays of gum disease show radiographic bone loss performed in our Gum Disease Treatment office.
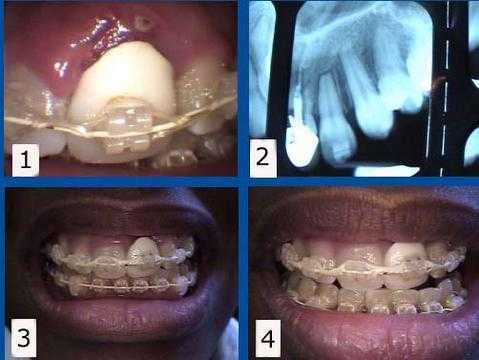
Orthodontic teeth braces complication. 1) & 2) This patient presented with a failing tooth #9 under an unattractive dental crown. The dental x-ray radiograph shows the extent of the tooth damage. The #9 tooth root was then extracted from under the tooth crown to allow the gum and bone to heal eight months before the completion of her dental braces. 3) & 4) This rootless tooth crown #9 is being held in place only by the orthodontic bracket and wire. This patient preferred to keep this unattractive crown during her orthodontic treatment to minimize simultaneous cosmetic changes, but a cosmetic temporary dental crown could also have been used during this time. A dental implant will be placed by the Oral Surgeon about three months following the tooth extraction. The second stage dental implant connection will coincide with the braces removal by the Orthodontist.

This periapical dental radiograph x-ray shows widening of the periodontal ligament space – PDL space – especially noticeable around the upper lateral incisor – associated with orthodontic tooth movement – teeth braces. This will return to normal in subsequent dental xrays following the completion of tooth movement.
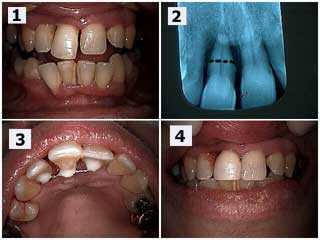
The patient’s chief complaint was that the upper right central incisor tooth (#8) was very loose and she wanted to try to save it. Pictures and dental radiograph x-ray. 1) Upper right central incisor (#8) has extruded and moved labially – toward the lip – and a diastema – tooth gap space – has occurred. 2) Radiographic xray view shows severe bone loss. The black dotted line shows the location for a potential root resection if necessary. Scaling and root planing was performed after the teeth splint was placed and the patient will return in three months for the Periodontist to reevaluate periodontal healing and the potential need for the root resection. 3) Palatal photo of the dental splint between teeth #’s 7 – 9. 4) Post-op picture. Same day. Notice the diastema teeth space was closed with dental bonding to hide the splint and the incisal edge of #8 was shortened.
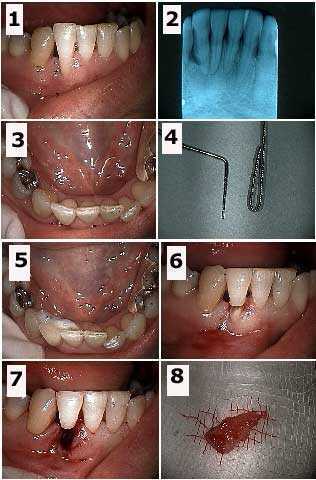
How to pictures with periapical x-ray. Tooth extraction of the root of a hopeless tooth #26 and teeth splinting the coronal portion of this tooth to the adjacent teeth in a 40 year-old female. 1) – 3) Initial photos and radiographic diagnosis. Note the extent of the bone loss seen in the xray. 4) The wire used for the splint next to a perio probe. The wire is doubled to prevent the tooth from rotating around it after placement. 5) The splint bonded to the lingual surfaces of teeth #’s 25 and 27. 6) Initial preparation through the mid-length of the tooth. 7) Following extraction of the root. 8) The extracted tooth root. This patient has already been through two rounds of root planing and scaling. After healing of this extraction site she will then have an apically positioned flap periodontal surgery and then possibly a graft to build up this area. It is expected that some other method for tooth replacement will be utilized following this periodontal therapy.

Clinical and radiographic diagnosis of severe gum disease. Treatment of a periodontally involved upper left central incisor tooth #9. 1) & 2) Pre-operative photograph and radiograph x-ray. Note the angular bony defect in the xray. The patient reported that the tooth was getting longer and that he never previously had the tooth gap space between his two front teeth. 3) Palatal photo of the dental splint placed between teeth #’s 8 & 9. 4) Post-operative view one hour later. Dental bonding was placed between the teeth to close the tooth space and it also hides the palatal splint. The incisal edge of #9 was shortened and the occlusion teeth bite was checked and adjusted for fremitus. Scaling and root planing was next performed by the dental hygienist and the patient scheduled for a three-month periodontist reevaluation.
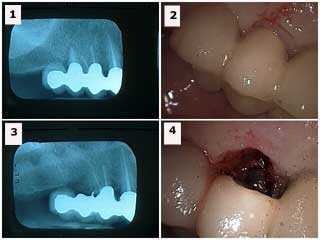
Tooth root resection from under a large porcelain fused to metal dental bridge. 1) Radiographic x-ray diagnosis shows the distal tooth abutment with an endo-perio lesion. 2) Labial photo of the same tooth. 3) Radiograph xray following tooth root resection (the metal chad in the area of the extracted abutment was later removed). 4) Labial image following extraction. This area could be filled in with dental bonding after wound healing. The occlusion teeth bite on the distal cantilever was reduced. It opposed a lower full arch bridge so that supraeruption was not a concern. Treatment options include: i) sectioning and removal of the distal cantilever, ii) dental implants, or iii) reevaluate over time with the patient informed to reduce function in this area. This teeth bridge has remained stable to nine years since this dental treatment.
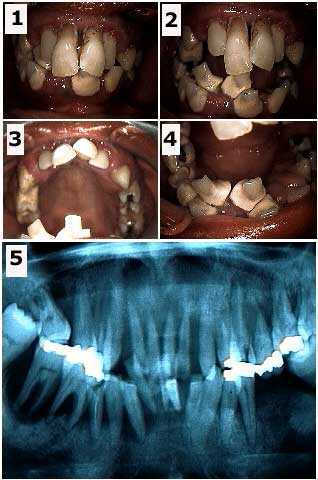
Full mouth dental reconstruction of a phobic 36 year-old female. Initial visit photos and panoramic x-ray. It is important to determine what teeth, if any, may be saved at least temporarily. It is easier for a patient to emotionally adjust to a provisional temporary fixed dental prosthesis that has at least some amount of retention provided by natural teeth abutments. With dental fear patients it is wise to start radiographic diagnosis using a panoramic xray rather than taking many individual periapical and bitewing x-rays because it is easier for the patient. One may need the detail offered by these xrays at a later time perhaps when the patient feels more comfortable.
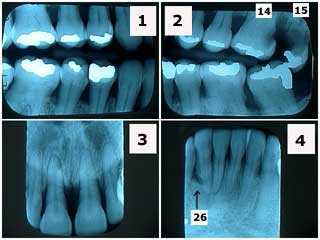
These periapical and bitewing x-rays show severe periodontal gum disease in a 40-year-old dental fear phobia patient. Note in the xrays the significant horizontal bone loss and the lack of radiographic calculus. Tooth #26, adjacent to the vertical bony defect, is probably hopeless. This patient was treated with two rounds of scaling and root planing then periodontist reevaluation. Tooth #15 was extracted and #14 had root canal treatment for tooth pain and a dental crown
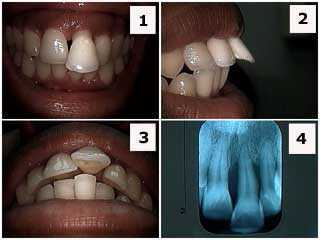
Patient presented with her upper left central incisor flared labially. 1) Front photo. 2) Side photo. 3) Occlusal image. 4) Dental x-ray radiograph. The patient, who was in her twenties, was informed about the severe periodontal condition and that the prognosis for this tooth was guarded at best. She was informed that a thorough Periodontist examination was needed. Orthodontics teeth braces is contraindicated – not recommended – here because of the severe periodontal gum disease. If the patient accepts treatment on a tooth with a guarded prognosis, it could include: scaling and root planing, open flap debridement if necessary, root canal therapy and a dental crown for esthetics and possibly a teeth splint. Treatment, otherwise, could include just scaling and root planing and incisal adjustment. Patients typically prefer to save teeth as long as the periodontal infection in the gums can be controlled.
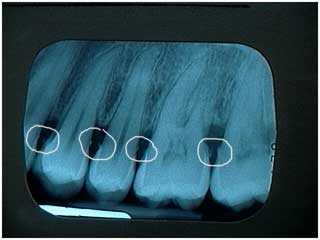
Radiographic calculus. Calculus is plaque that becomes hardened by absorbing salivary calcium and then becomes evident on x-rays. It usually indicates the chronic presence of plaque and is not healthy. A dental prophylaxis teeth cleaning with the dental hygienist and then possibly scaling and root planing is usually indicated. The hygienist should look at each dental xray radiograph to see the location of the calculus during the periodontal treatment. This is frequently followed by a Periodontist evaluation.

Radiographic calculus. Dental calculus is plaque that becomes hardened by absorbing salivary calcium and then becomes evident on radiographs x-rays. It usually indicates the chronic presence of plaque and is associated with many diseases of the gums. A teeth cleaning, and then possibly scaling and root planing is usually recommended followed by periodontal reevaluation with a Periodontist. A dental xray is very important part of periodontal diagnosis.
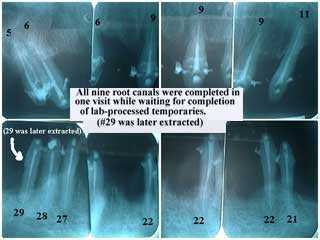
Radiographic x-ray series of a smile makeover. This root canal treatment on nine teeth was performed by an Endodontist in one visit while the Cosmetic Dentist and Dental Laboratory Technician created the lab-processed provisional temporary dental crowns. In these periapical x-rays note that the root canal filling material extends to the tooth root apex. Tooth #29 was later extracted.
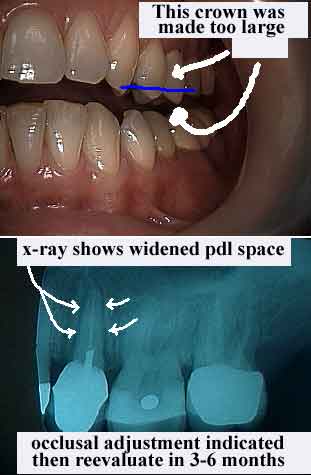
Radiographic x-ray evidence of Occlusal Trauma. Photo and xray. Note in the radiograph the widening periodontal ligament space. Occlusal adjustment – bite adjustment – should be considered a part of periodontal therapy.

Occlusal periodontal – combined teeth bite and gum – problems. It is common for middle-aged patients to visit with a chief complaint that the upper front have moved and that a tooth gap space has developed. A dental radiograph or series of x-rays is needed for initial diagnosis. Fremitus – vibration movement – of an upper front tooth upon closing the teeth – biting – is also commonly seen and needs to be corrected. Notice the deep bite occlusion. Consider lower anterior incisal adjustment. The Periodontist will probably recommend periodontal scaling and root planing and then gum surgery in the upper anterior from the palatal. Following gum healing consider either upper orthodontic movement – teeth braces – to bring these teeth back palatally or cosmetic dentistry. Radiographic interpretation of a periapical x-ray is important in dental diagnosis. Many dentists unfortunately treat patients without xrays.
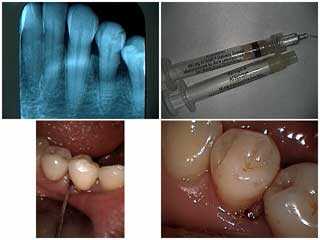
Periodontal gum disease symptoms diagnosis and treatment based upon a dental x-ray radiograph and clinical examination. 1) This patient presented with an isolated moderate periodontal pocket. A full mouth series of dental xrays confirmed there were no other areas of bone loss. 2) In this case, a conservative site-specific periodontal treatment was used with doxycycline gel – Atridox. 3) The Periodontist inserted the gel into the periodontal gum pocket via a canula and excess is pushed into the pocket with a moistened scaler without local anesthesia. 4) Final placement. How to gum disease treatment pictures and dental xray.