Photos and X-rays on a tooth abscess from infection causes pain or swelling created in our Root Canal office.
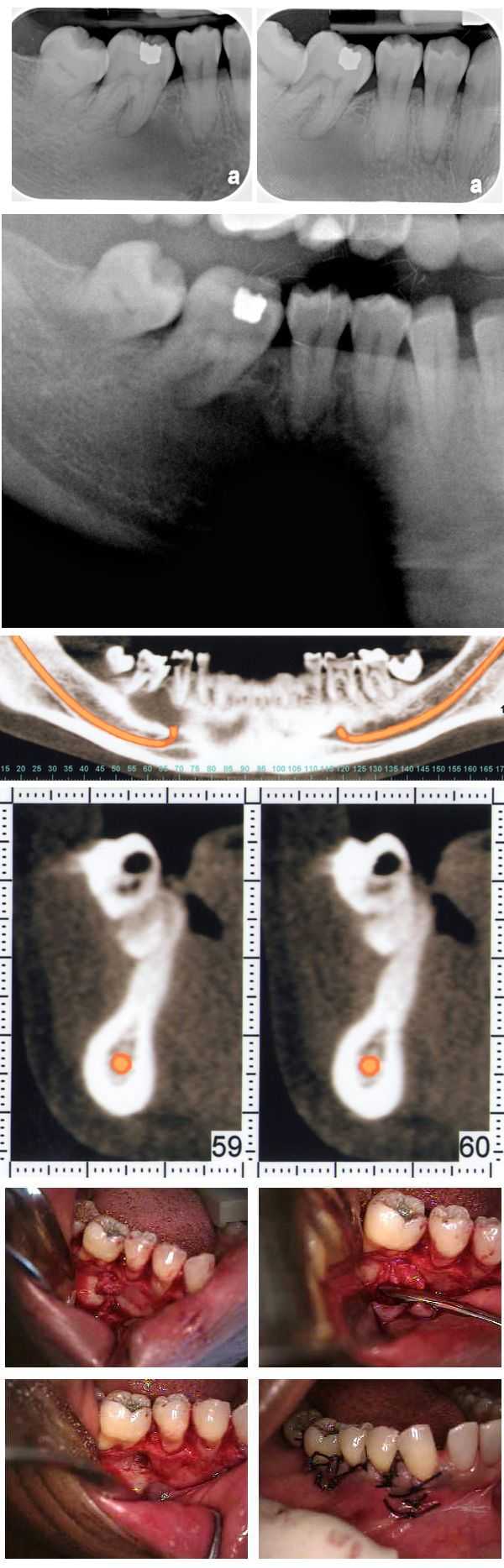
An atypical bone pattern was noted on a 46 year old female during routine dental x-rays. A Panoramic x-ray also showed something unusual. A subsequent oral surgeon exam revealed no expansion of lingual or buccal plates. The teeth have not moved for many years though #30 was extracted many years prior. A moderate depression was noted on the buccal aspect of teeth #’s 29 & 30. The patient exhibited mild discomfort in this area upon palpation. A CAT scan confirmed the bone loss and an exploratory surgery was performed. The clinical impression was that of a lateral periodontal cyst. The pathology report showed it to be mildly inflamed fibrous tissue. Note the importance of careful evaluation of bone patterns in regular dental x-rays.
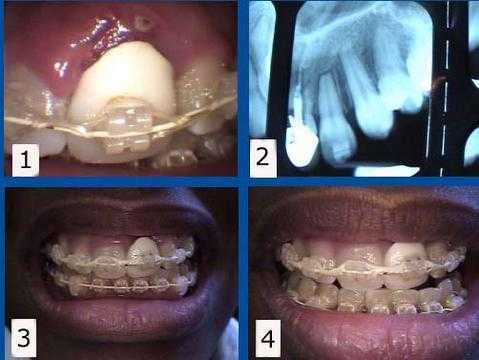
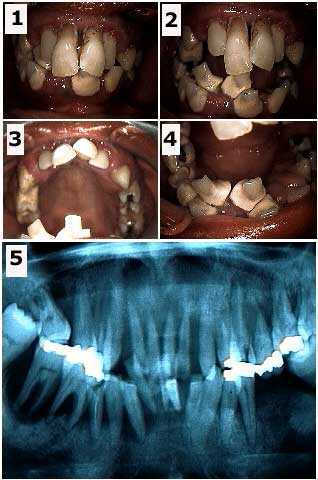
Orthodontic complications. 1) & 2) This patient presented with a failing tooth #9 under an unattractive dental crown. This tooth was maintained for one year while her teeth were being orthodontically aligned. The #9 tooth root was then extracted from under the crown to allow the gum and bone to heal with about eight months remaining to complete her braces. 3) & 4) This rootless crown #9 is being held in place only by the orthodontic bracket and wire. This patient preferred to keep this unattractive crown during her ortho treatment to minimize simultaneous cosmetic changes, but a cosmetic temporary tooth crown could also have been used during this time. A dental implant will be placed about three months following the extraction. The second stage implant connection will coincide with the braces removal.
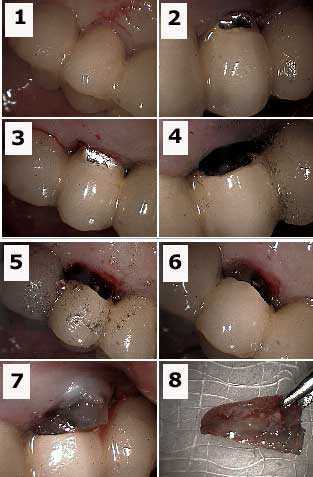
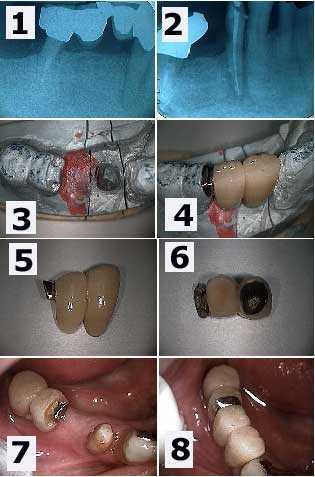
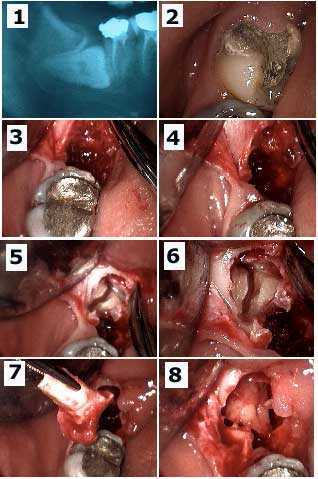
Pictures showing technique for tooth root resection from under a porcelain fused to metal bridge.
1) Labial photo of a tooth abutment with an endo-perio lesion – this is a combined root canal and gum infection. 2) & 3) Initial preparation into porcelain crown with a diamond bur. 4) Labial photo showing preparation – i.e., drilling. The metal portion of the dental bridge is prepared with a steel bur. 5) Palatal view showing preparation. 6) Labial view showing the tooth root under the porcelain (gutta percha is visible in the tooth root). 7) Tooth root being extracted. The occlusal height of this root must first be reduced to allow it to exit. 8) The extracted tooth root.
1) Labial photo of a tooth abutment with an endo-perio lesion – this is a combined root canal and gum infection. 2) & 3) Initial preparation into porcelain crown with a diamond bur. 4) Labial photo showing preparation – i.e., drilling. The metal portion of the dental bridge is prepared with a steel bur. 5) Palatal view showing preparation. 6) Labial view showing the tooth root under the porcelain (gutta percha is visible in the tooth root). 7) Tooth root being extracted. The occlusal height of this root must first be reduced to allow it to exit. 8) The extracted tooth root.

Acute periodontal gum abscess that was not painful. This patient had not been to the dentist for over two years. The x-rays look normal and the patient felt no pain from this gum infection. He received a dental cleaning and was placed on a chlorhexidene mouthwash. He was rescheduled for root planing and scaling and then further reevaluation.
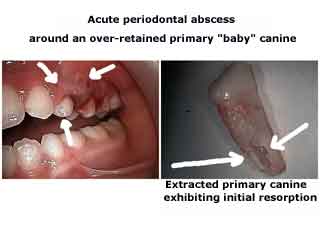
Acute periodontal abscess around an over-retained primary baby canine tooth. The extracted primary canine is also shown.
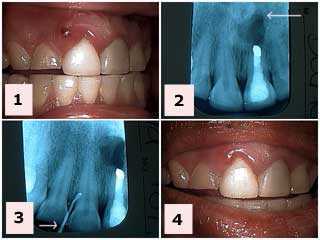
Acute periodontal abscess that was painful. 1) This patient presented with this fistula between tooth #’s 7 & 8. Tooth #’s 8 & 9 had acrylic laminates placed about two years ago. Her general dentist had performed a gingivectomy last year to attempt to treat the occasional swelling of the gum in this same area. 2) The radiograph of tooth #9 shows a healed apicoectomy from 12 years ago that is not related to the current problem. 3) A gutta percha point was placed in the fistula and radiographed to see where it leads. It stayed at the coronal gingiva probably around the margin of the laminate. The patient was put on tetracycline for a week. [This is not a recommendation for everybody!] 4) Reevaluation two days later shows improvement in symptoms and gingival inflammation. An evaluation and treatment of the laminate margin will occur following resolution of the acute condition.

Acute periodontal abscess that caused pain. This patient presented with this painful gum fistula between teeth #’s 7 & 8. Tooth #’s 8 & 9 had acrylic laminates placed about two years ago. Her general dentist had performed a gingivectomy last year to attempt to treat the occasional swelling of the gum in this same area. A gutta percha point was placed in the fistula and radiographed to see where it leads. It stayed at the coronal gingiva probably around the margin of the laminate. The patient was put on tetracycline for a week. [This is not a recommendation for everybody!]. Reevaluation two days later shows improvement in symptoms and gingival inflammation. An evaluation and treatment of the laminate margin will occur following resolution of the acute condition.
How to pictures. Cervical decay – gumline cavity – and root canal infection around a lower right first premolar. 1) A large radiolucency is seen in the x-ray. Note the distal abutment is the distal root of a first molar tooth following hemisection. 2) Following root canal therapy. The cervical decay can now be seen more easily. 3) The working model showing the preparation of the mesial part of the distal two-unit bridge. This preparation will allow rigid connection to the new anterior bridge being made. 4) The new bridge section in place on the working model. 5) & 6) Two views of the new bridge showing the distal attachment. 7) An intraoral view which mirrors the working model view seen in 3). 8) The final result. This patient was content to see the gold occlusal rest. Otherwise, it could have been hidden under porcelain.
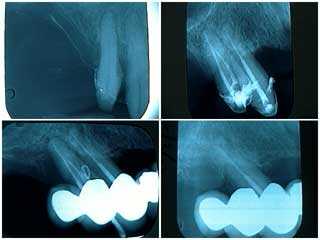
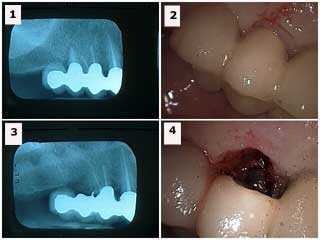
Radiographs of a failing distal abutment tooth in a one year old oral reconstruction. 1) Pre-operative x-ray. 2) Following root canal therapy, root planing and open debridement. 3) Gutta percha placed into a periodontal abscess one year later. 4) Following root planing, targeted antibiotics and extraction. The roots of this extracted tooth were fused. This patient was scheduled for a three month recall; she did not return for eight months following her first three month recall visit. The periodontal abscess was readily apparent at this time. It is suggested that reconstruction patients are treated, not cured, and that they must be closely supervised. Patients need to be acutely aware of the need for frequent recall visits. It is possible that earlier diagnosis and intervention might have prevented the loss of this tooth.

How to technique for extraction of a failing distal abutment tooth under a fixed, porcelain fused to metal reconstruction dental bridge. 1) Upper first premolar with probing to the apex. 2) Horizontal sectioning through tooth to separate it from the bridge. You need to reduce enough of the remaining tooth root to elevate it while under the bridge. 3) Tooth socket after tooth removal. 4) Extracted tooth root. The gingival surface of the newly created pontic could be bonded after primary healing has occurred.
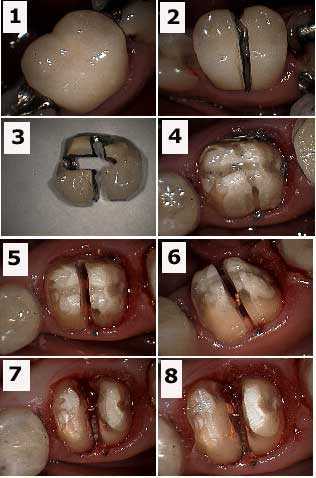
Dental crown removal and root resection – hemisection. 1) Pre-op tooth crown photo. 2) Initial preparation through crown. 3) Crown after removal. 4) Tooth after crown removal. 5) Preparation through composite core. 6) Gutta percha (orange color) is visible. 7) Hemisection completed. 8) Gutta percha is exposed and requires more composite to seal it within the tooth after crown lengthening periodontal gum surgery.
Root resection from under a porcelain fused to metal bridge. 1) Radiograph showing the distal abutment with an endo-perio lesion. 2) Labial view of the same tooth. 3) Radiograph following resection (the metal chad in the area of the extracted abutment was later removed). 4) Labial view following extraction. This area could be filled in with bonding after healing. The occlusion on the distal cantilever was reduced. It opposed a lower full arch bridge so that supra-eruption was not a concern. Treatment options include: i) sectioning and removal of the distal cantilever, ii) implants, or iii) reevaluate over time with the patient informed to reduce function in this area.
Full mouth reconstruction of a phobic 36 year-old female. Initial visit. It is important to determine what teeth, if any, may be saved at least temporarily. It is easier for a patient to emotionally adjust to a temporary prosthesis that has at least some amount of retention provided by natural tooth abutments. The teeth chosen were #6, 11, 22 and 28. The decision to fabricate a removable immediate partial denture, rather than a fixed lab-processed temporary bridge, was determined by the particular weakness of tooth #28. The patient was informed that the immediate prosthesis was to be used for the healing phase and that the four remaining abutments, particularly #28, might be subsequently extracted. Photo #2 of 4.

Full mouth oral reconstruction of a 36 year-old female who suffered from dental anxiety. Before and after photo shows the initial result: two visits. Photo #1 of 4.
Extraction of a horizontally-impacted lower wisdom tooth and a very decayed second molar. The patient was in a lot of pain. 1) Pre-op x-ray. 2) Tooth #31 had a temporary filling in it. 3) – 4) After removal of the crown of #32 showing the residual empty socket. 5) – 6) Minimal flap reflected to show exposure of the roots of #32 with sectioning. 7) Removal of first root. 8) Second root brought forward in socket and ready for removal.
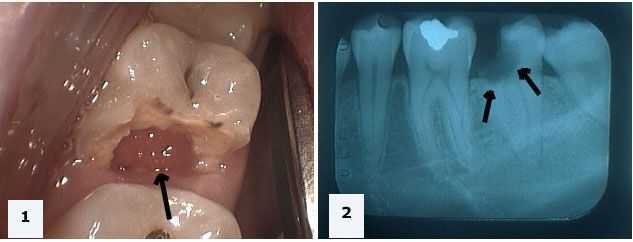
A hopeless tooth that should be extracted. 1) Photo of tooth #18 showing gum tissue growing into the space previously occupied by tooth structure. 2) X-ray showing extensive decay extending below the level of the jawbone.